The Devastating Reality of Pressure Ulcers: A Call to Action for Medical Professionals
Pressure ulcers, also known as bed sores or pressure injuries, are a preventable and treatable condition that affects patients in long-term care facilities, hospitals, and rehabilitation centers. These lesions can cause significant pain, discomfort, and even life-threatening complications, making it essential for medical professionals to take proactive steps in prevention and management. In this article, we will delve into the graphic images of pressure ulcers, their causes, symptoms, risk factors, and effective prevention strategies, as well as the latest treatment options and rehabilitation techniques.
Understanding Pressure Ulcers
Pressure ulcers are areas of damaged skin that occur when pressure, friction, or shear forces cause tissue damage, leading to inflammation and potentially, infection. They can affect anyone, but certain populations, such as older adults, people with limited mobility, and those with neurogenic disorders, are at higher risk of developing pressure ulcers.
Types of Pressure Ulcers
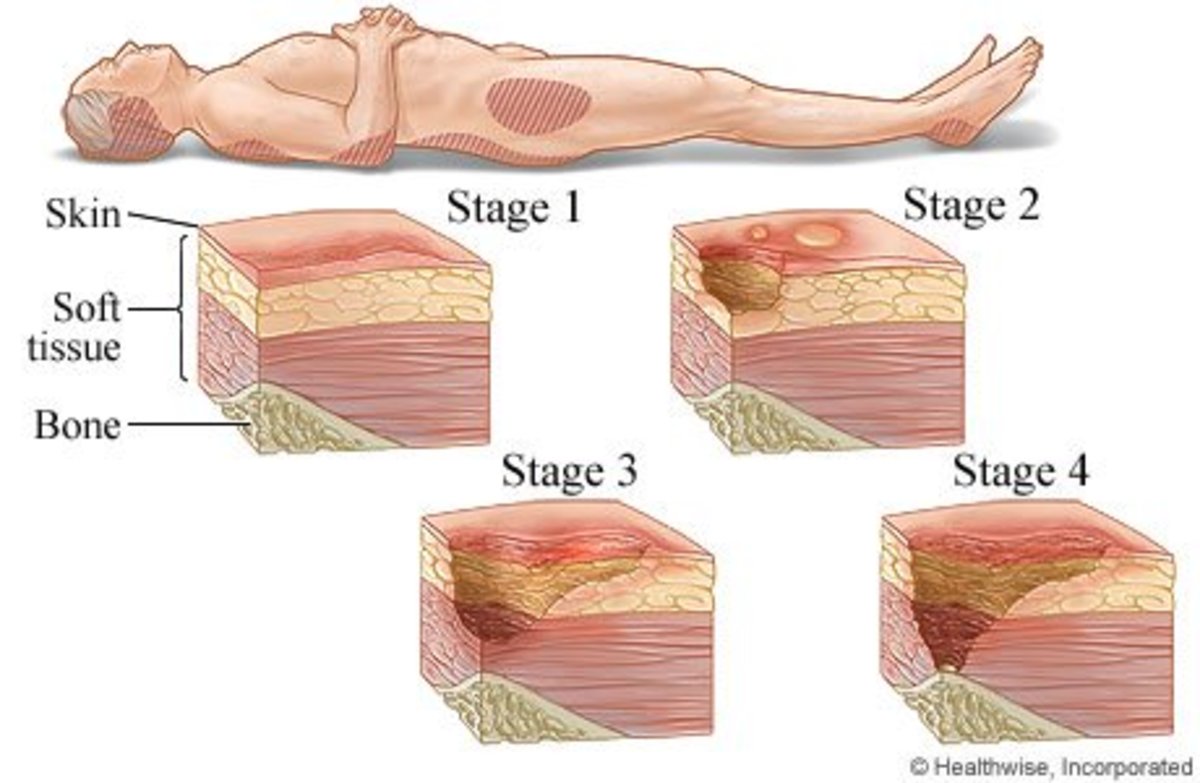
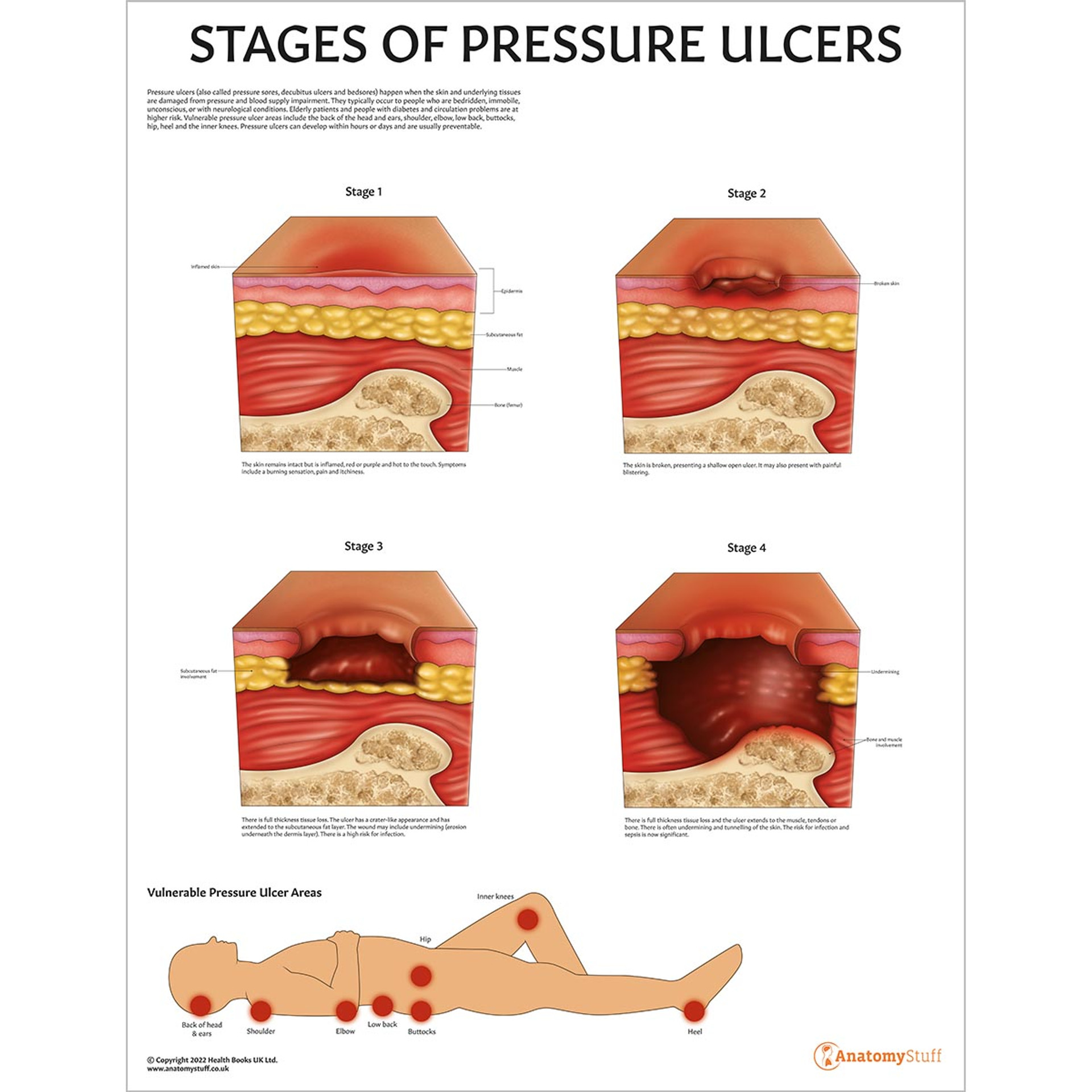
There are four stages of pressure ulcers, each with distinct characteristics:
- Stage 1: Non-blanchable erythema (redness without blanching) - a warning sign of potential tissue damage
- Stage 2: Partial-thickness skin loss - visible skin loss with exposed nerve endings
- Stage 3: Full-thickness skin loss - significant skin loss with exposed muscle and bone
- Stage 4: Full-thickness skin and tissue loss - severe tissue damage with exposed bone and muscle
Causes and Risk Factors
Pressure ulcers can be caused by various factors, including:
- Prolonged immobility: Lack of movement can lead to increased pressure on certain areas of the body
- Poor circulation: Reduced blood flow can impair the delivery of oxygen and nutrients to tissues
- Friction and shear: Rubbing and sliding of skin against surfaces can cause tissue damage
- Neurogenic disorders: Conditions such as stroke, spinal cord injury, or multiple sclerosis can increase the risk of pressure ulcers
- Malnutrition: Inadequate nutrition can impair wound healing and tissue repair
Symptoms and Signs
The early signs of pressure ulcers may be subtle, but as the condition progresses, they can become more apparent:
- Redness and swelling: Early warning signs of pressure ulcer development
- Pain and tenderness: Patients may experience discomfort or pain when pressure is applied
- Open wounds: Visible open sores or ulcers
- Tissue damage: Visible signs of tissue damage, such as exposed bone or muscle
Effective Prevention Strategies
Prevention is key to avoiding pressure ulcers. Some effective strategies include:
- Moving patients regularly: Gentle turning and repositioning can help distribute pressure evenly
- Using pressure-redistributing devices: Products such as foam wedges and gel cushions can help redistribute pressure
- Maintaining good hygiene: Keeping the skin clean and dry can help prevent infections
- Providing proper nutrition: Ensuring adequate nutrition can support wound healing and tissue repair
Treatment Options
Treatment options for pressure ulcers depend on the stage and severity of the condition:
- Topical treatments: Creams, gels, and ointments can help promote healing and tissue repair
- Debridement: Removing dead tissue and debris can help promote healing
- Negative pressure wound therapy: A type of wound vacuum that can help remove fluid and debris
- Surgical interventions: In severe cases, surgical intervention may be necessary to remove damaged tissue and repair damaged structures
Rehabilitation Techniques
Rehabilitation techniques can help improve the function and mobility of patients with pressure ulcers:
- Physical therapy: Gentle exercises and stretches can help improve range of motion and strength
- Occupational therapy: Assisting patients with daily activities and tasks can help promote independence
- Speech therapy: Addressing communication and swallowing difficulties can help patients regain functional abilities
- Pain management: Effective pain management can help reduce discomfort and promote healing
Preventing Future Occurrences
To prevent future occurrences of pressure ulcers, medical professionals should:
- Monitor patients regularly: Regular assessments can help identify high-risk patients and prevent ulcer development
- Implement prevention strategies: Using pressure-redistributing devices, maintaining good hygiene, and providing proper nutrition can help prevent pressure ulcers
- Educate patients and families: Raising awareness about pressure ulcers and the importance of prevention can help promote healthy behaviors
- Develop personalized care plans: Creating individualized care plans can help address the unique needs and risk factors of each patient
Pressure ulcers are a preventable and treatable condition that requires a multidisciplinary approach. By understanding the causes, symptoms, and treatment options, medical professionals can take proactive steps to prevent and manage pressure ulcers, ultimately improving patient outcomes and quality of life.
Uday Chopra
Janice Nichole Rivera
Sabrina Carpenter Height Ft
Article Recommendations
- Sahara Rose Real Name
- Kaitlyn Krems Fans
- Shri
- When A Guy Hugs You Multiple Times
- Gina Wapd
- Taylorwift Height And Weight
- Julesari
- Megyn Kelly Children
- Joyymei
- John Pinette